Dr. Richardson and Dr. Memsic are two of the top breast surgeons in Los Angeles, using innovative techniques to create excellent clinical and aesthetic outcomes.
Schedule a Visit
Bedford Breast Center
436 N Bedford Dr, Ste 308
Beverly Hills, CA 90210
Phone: (310) 278-8590
Monday – Friday: 9 a.m.– 5 p.m.
Prophylactic Mastectomy
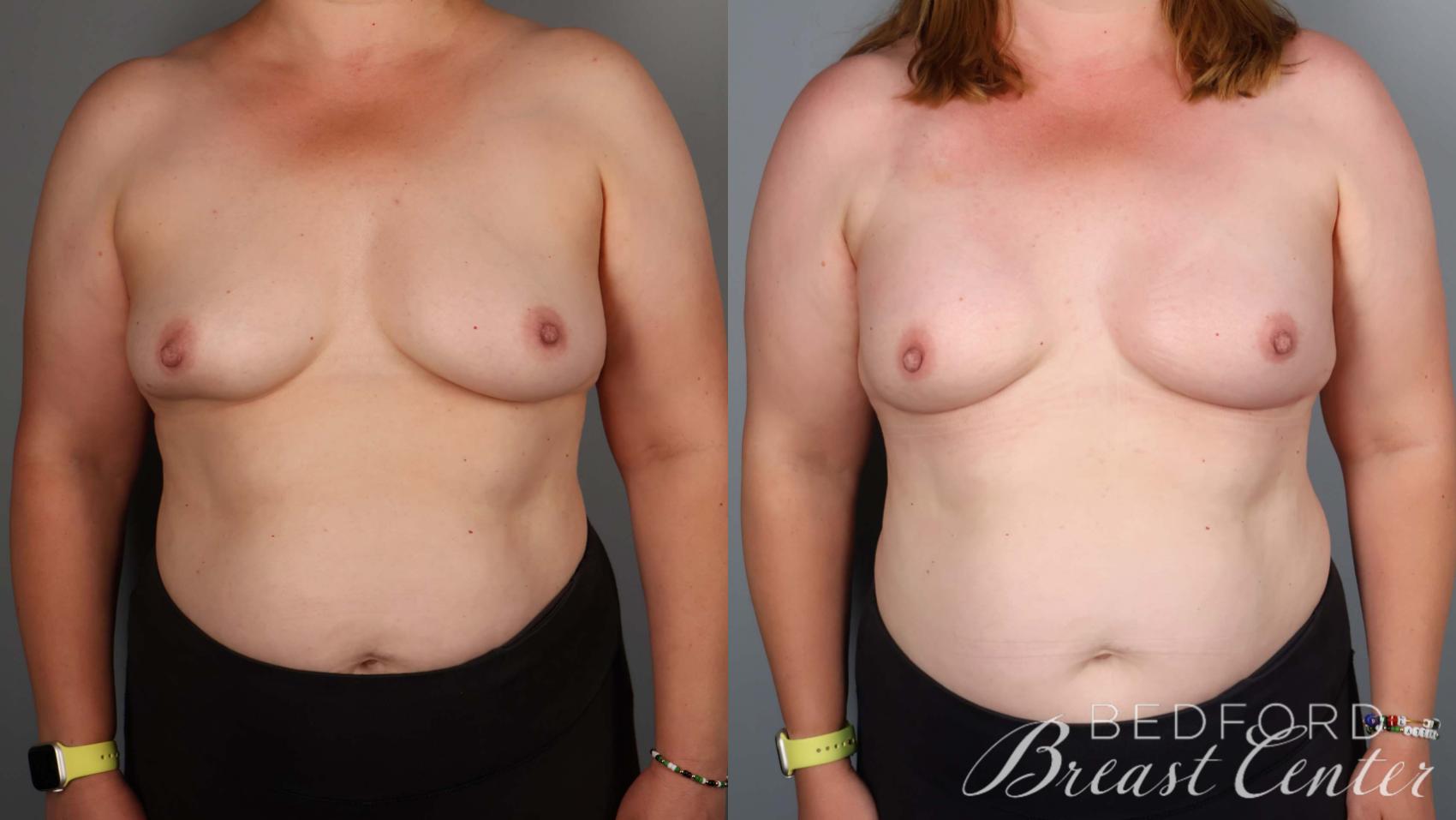
Prophylactic mastectomy, also known as preventive mastectomy, involves the removal of one or both breasts to reduce the risk of developing breast cancer if you’re at high risk. At Bedford Breast Center in Beverly Hills, we understand the difficult choices involved in considering prophylactic mastectomy surgery. Our goal is to help educate and support our patients from the Greater Los Angeles area, Orange County, and Ventura County as they make these decisions.
What Is Prophylactic Mastectomy?
The word “prophylactic” means “intended to prevent disease.” A prophylactic mastectomy is the preemptive surgical removal of the breast tissue to minimize breast cancer risk for women at high risk of developing the disease.
Who Is a Good Candidate for Prophylactic Mastectomy?
Women with a family history of breast cancer or specific genetic markers face a significantly higher risk. Other factors that may contribute to an increased risk include a history of cancer in one breast, a strong family history of breast or ovarian cancers, dense breast tissue, exposure to radiation therapy at an early age, and certain gene mutations.
Being identified as high risk for breast cancer doesn’t mean you will develop the disease, but it indicates that your risk is significantly higher than women with average risk. By understanding your risk level, you can better evaluate your options and make informed decisions.




How Effective Is Prophylactic Mastectomy?
Prophylactic mastectomy can be highly effective in reducing the risk of breast cancer, potentially decreasing breast cancer risk by up to 90% in women with a very high risk. The degree of risk reduction varies depending on individual factors, such as family history and genetic markers. For instance, individuals with a BRCA1 mutation and a first-degree relative with breast cancer may face a 55-65% risk of developing breast cancer by age 70. However, this risk decreases to as low as 5% after undergoing prophylactic mastectomy. However, it is important to note that while the procedure significantly reduces the risk, prophylactic mastectomy cannot eliminate the possibility of developing breast cancer.
What Are the Alternatives to Prophylactic Mastectomy?
Alternatives to prophylactic mastectomy include lifetime surveillance involving periodic mammograms, physical exams, and ultrasounds, with immediate treatment if abnormalities are detected. Anti-hormone therapy medications such as tamoxifen can decrease the risk of breast cancer by nearly 50% in high-risk patients, but the potential side effects should be considered.
Additional alternatives include combining MRIs with mammograms for enhanced detection, prophylactic removal of the ovaries to decrease the risk of breast and ovarian cancer, and maintaining a healthy lifestyle through weight management, regular exercise, limited alcohol consumption, and avoiding hormone therapy during menopause.
“I am one week post-op from my preventative double mastectomy with Dr. Richardson and I couldn’t be any happier! Who would have thought that I would have BETTER boobs after a mastectomy? Well, Dr. Richardson and Dr. Cassileth gave me perfect breasts. Undergoing a double mastectomy is no easy journey- but Dr. Richardson was there the whole way cheering me along and guiding me. I love her! They have an amazing team (shout out to Nora!) – they are so kind and you feel so welcome and safe there. If you are thinking about having a double mastectomy – I without a doubt would recommend Dr. Richardson. I can’t express how amazing she is and how happy I am. I feel beautiful and whole again.”
Sara A. – Yelp
What Prophylactic Mastectomy Options Are Available?
Prophylactic mastectomy options may include a simple mastectomy, a modified radical mastectomy, a skin-sparing or nipple-sparing mastectomy, or breast-conserving surgery.
- A simple mastectomy involves the removal of most of the breast tissue without removing the lymph nodes. It is also referred to as a total or radical mastectomy.
- A modified radical mastectomy is the most common prophylactic surgery, removing as much breast tissue as possible while preserving the chest wall muscles.
- Skin-sparing or nipple-sparing mastectomy involves the removal of all breast tissue while preserving healthy skin and nipples.
- Breast-conserving procedures, such as the innovative SWIM, Goldilocks, or direct-to-implant techniques developed by Bedford Breast Center surgeons, reconstruct the breast as a second stage of mastectomy surgery and provide excellent cosmetic outcomes. This 2-stage approach eliminates the need for tissue expanders and multiple surgeries associated with traditional reconstruction techniques.


- No Compression - Comfortable, pain-free imaging
- Open Design - Won't trigger claustrophobia
- Ideal for Dense Breasts - Advanced detection with contrast
- Fast Results - Complete scan in under 10 minutes
Vera Scan with contrast provides enhanced detection comparable to MRI, delivering precise, accurate diagnosis in a fraction of the time.
Call (310) 278-8590 to reserve your appointment.
Is Vera Scan Right For You? Take The QuizHow Is Prophylactic Mastectomy Performed?
Surgical techniques vary depending on whether concurrent breast reconstruction is desired and the chosen reconstruction technique. Prophylactic mastectomy is performed under general anesthesia.
Our surgeons perform mastectomy through a small incision along the inframammary fold beneath the breast. The breast tissue is then carefully removed while preserving the chest wall muscles. The blood vessels and lymphatic vessels supplying the breast tissue are identified and ligated. In a prophylactic mastectomy, the nipple is not typically removed but may be repositioned on the breast mound.
Small drains may be placed in each breast to remove fluid for several days. The incisions are closed with sutures, which may dissolve on their own or be removed at the first postoperative visit.
“The experience of my first appointment was a game changer — BRCA patients who have dealt with brash or pushy doctors know how sensitive and scary new appointments can be. Dr. Richardson was SO nice from the get go. I had always wanted to do a preventative mastectomy and reconstruction, and Dr. Richardson helped explain their one-stage process (I didn’t even know it was a possibility!) in a way that made sense. She referred me to Dr. Killeen, next door at Cassileth Plastic Surgery, and I ultimately chose them as my team, doing the surgery just a couple of months later.”
Kelli L. – Yelp
What Is the Recovery From Prophylactic Mastectomy Like?
It is normal to experience some pain; it is usually at its most intense within 24 to 48 hours after surgery. Pain medication can help manage discomfort, which gradually improves within a few days. Some patients may experience a dull ache in the chest wall for up to 6 weeks following the procedure.
Surgical drains are removed a few days after surgery, depending on the amount of fluid collected. Your health care team will provide specific instructions on drain care. Showers are usually permitted 48 hours after drain removal or as your doctor advises.
The breast surgeons at Bedford Breast Center in Beverly Hills are innovative physicians who provide compassionate, personalized patient care. Our world-class facility serves patients from throughout Los Angeles, Southern California, and nationwide. To learn more about our center and if prophylactic mastectomy is the right option for you, call us at (310) 278-8590 or contact us using the online form to schedule an appointment.
Curious if your procedure is covered by insurance? Bedford Breast Center has partnered with a specialized billing service to help you maximize your insurance benefits. Click here to take a short quiz and find out if you qualify.