Dr. Richardson and Dr. Memsic are two of the top breast surgeons in Los Angeles, using innovative techniques to create excellent clinical and aesthetic outcomes.
Schedule a Visit
Bedford Breast Center
436 N Bedford Dr, Ste 308
Beverly Hills, CA 90210
Phone: (310) 278-8590
Monday – Friday: 9 a.m.– 5 p.m.
Nipple-Sparing Mastectomy
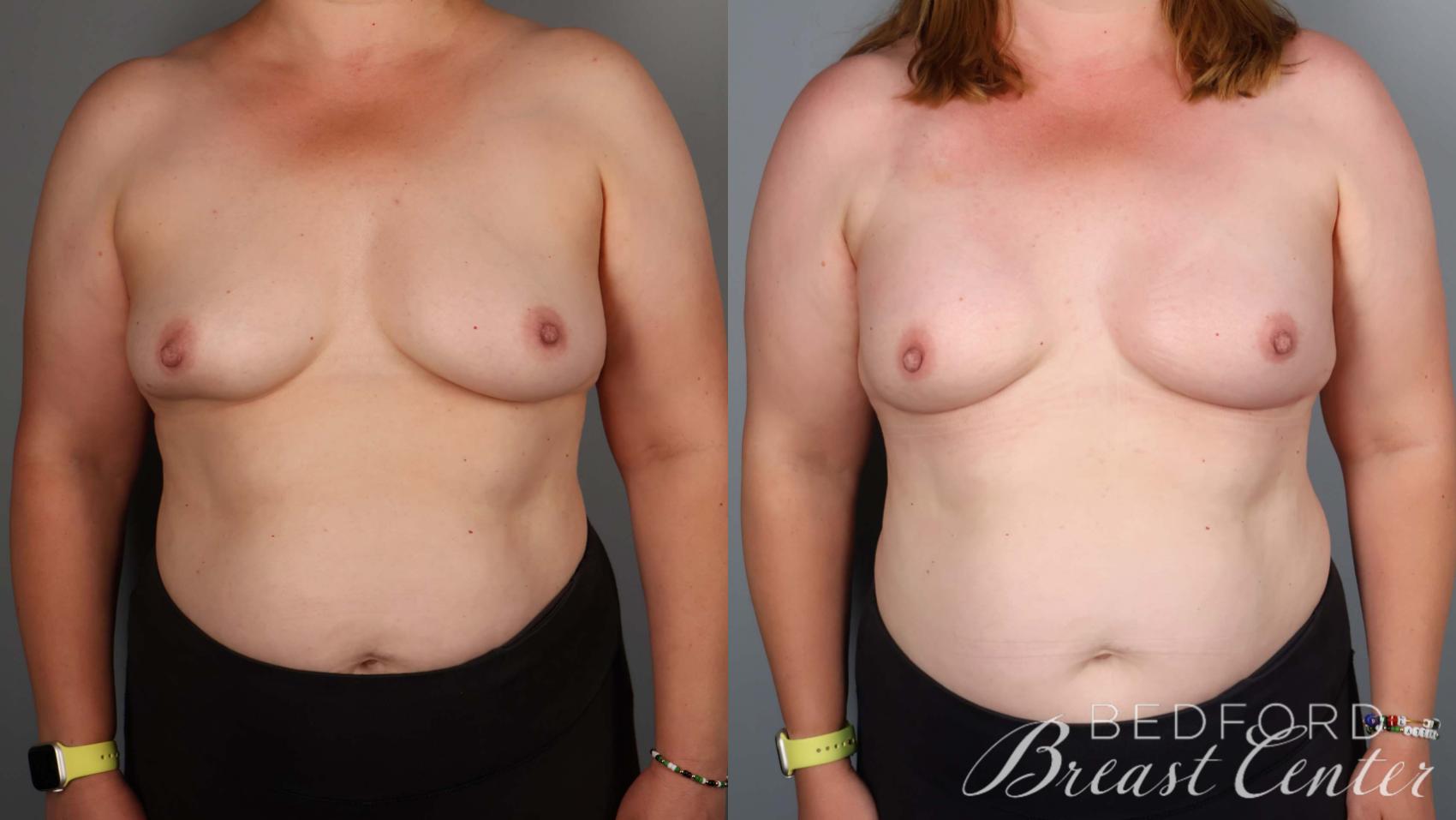
At Bedford Breast Center in Beverly Hills, we prioritize both health and beauty in breast cancer treatment. Our surgeons’ unrivaled skill with nipple-sparing mastectomy and reconstruction is one reason many women in the Greater Los Angeles area, Orange County, and Ventura County choose us for their breast cancer surgeries. We can provide this advanced procedure to about 95% of women with breast cancer that has not spread to the nipple.
What Is Nipple-Sparing Mastectomy?
Nipple-sparing mastectomy involves removing cancerous breast tissue while preserving the nipple-areola complex. Unlike traditional mastectomy, which removes the nipple and areola, this procedure allows women to maintain a natural, aesthetically pleasing—even beautiful—appearance. Because of the technical difficulty of this technique, relatively few breast centers offer this option. Bedford Breast Center stands apart with our expertise and experience in nipple-sparing mastectomy in Los Angeles, boasting a complication rate of under 8%.
Studies have shown that preserving the nipple and areola does not compromise the cure rate of breast cancer. Nipple-sparing mastectomy actually reduces overall risk, lowers costs, and minimizes postoperative pain.
Who Is a Good Candidate for Nipple-Sparing Mastectomy?
Most women with breast cancer are candidates for nipple-sparing mastectomy, except when the nipple is involved with the tumor. Other factors, such as low nipple position or large breast size, may also contraindicate the procedure. Women with large breasts might be better suited to a SWIM mastectomy and reconstruction.




What Are the Advantages of Nipple-Sparing Mastectomy?
The technique offers several advantages:
- Aesthetic preservation: Nipple-sparing mastectomy allows for breasts that look natural and maintain their shape and size. The incision is strategically placed—hidden in the natural crease under the breast—resulting in minimal scarring.
- Improved sexual well-being: Studies have shown that women who undergo nipple-sparing mastectomy report higher levels of sexual well-being than those who opt for traditional mastectomy.
- Safety and efficacy: The procedure has proven to be as effective as traditional mastectomy in treating breast cancer. Studies have shown that nipple-sparing mastectomy patients have a slightly better survival rate during the critical 5-year postoperative period.
“I traveled from Las Vegas to California for surgery with Dr Richardson. I had been diagnosed with stage zero breast cancer and due to previous lumpectomies and tissue loss, I had to have a mastectomy. I had been told by another surgeon that I would lose my nipple and the incision would be across my breast. I was extremely happy to find out from Dr Richardson that I was a candidate for nipple sparing surgery with direct to implant reconstruction and an infra-mammary incision. Dr Richardson is very knowledgeable and confident and answered all of my questions, putting me at ease for surgery.”
Kerry G. – Google
How Is Nipple-Sparing Mastectomy Performed?
Bedford Breast Center’s skilled breast surgeons are experts in this technique. During the consultation, we carefully assess each patient’s eligibility for the procedure based on test results and individual factors. Here’s an overview of how nipple-sparing mastectomy is performed:
- Anesthesia: The procedure is performed under general anesthesia.
- Incision: The incision is made under the breast or in the underarm area, depending on the patient’s unique situation. This allows the breast surgeon to minimize visible scarring but still remove the cancerous tissue.
- Cancer removal: The breast surgeon safely removes cancerous breast tissue while leaving the nipple and areola intact. Unlike traditional mastectomy, where the nipple and areola are removed, NSM spares these important aesthetic aspects of the breast.


- No Compression - Comfortable, pain-free imaging
- Open Design - Won't trigger claustrophobia
- Ideal for Dense Breasts - Advanced detection with contrast
- Fast Results - Complete scan in under 10 minutes
Vera Scan with contrast provides enhanced detection comparable to MRI, delivering precise, accurate diagnosis in a fraction of the time.
Call (310) 278-8590 to reserve your appointment.
Is Vera Scan Right For You? Take The QuizWhat Is Recovery Like After Nipple-Sparing Mastectomy?
The recovery process varies depending on individual factors such as age and overall health. Some patients may spend 1 to 2 nights under expert nursing care for rest and recovery. Others may return home the same day, accompanied by a family member, after an observation period.
It is normal to experience some discomfort after the procedure. Patients are advised to avoid strenuous activities and focus on the provided physical therapy exercises.
Breast cancer treatment is more than just fighting the disease—it’s also about preserving emotional well-being and beauty. Nipple-sparing mastectomy can be game-changing, allowing you to maintain your natural appearance and confidence throughout your treatment.
Our breast surgeons at Bedford Breast Center in Beverly Hills are innovative physicians who provide compassionate, personalized patient care. Our world-class facility serves patients from throughout Los Angeles, Southern California, and nationwide. To learn more about our center and if nipple-sparing mastectomy is a good option for you, call us at (310) 278-8590 or contact us using the online form to schedule an appointment.
Curious if your procedure is covered by insurance? Bedford Breast Center has partnered with a specialized billing service to help you maximize your insurance benefits. Click here to take a short quiz and find out if you qualify.